We've talked a lot about diagnoses here on Shrink Rap. We've talked about how diagnoses are made, how valid they might be, how as labels they can be stigmatizing or damning in a person's life. We've talked about how they are used to guide treatment and how they are demanded to obtain reimbursement for care. What we haven't talked about is how they hang out over time.
When I see a patient for the first time, we meet for 2 hours, I take a full history, family members may come in, and subsequent to the appointment, I may talk with a past psychiatrist, a current primary care doc, and I may request old records that I will review. I take the information I have and I form a diagnosis. Is it the right diagnosis? Oh, who knows. I don't sit there with the DSM and read off a check list and some of it is art. The DSM diagnoses aren't science, they were voted on by a committee. I come close. Like what is the exact divide between Major Depression, recurrent, mild versus Major Depression, recurrent, moderate ? To the extent that it guides treatment, I care about getting it right, but sometimes the honest answer is I Don't Know. Or the patient comes to me after they have gotten well--- they are not currently having symptoms, but they are on medications which they say help, and they report that before they were on medications, they had symptoms consistent with Diagnosis X. If they are medications that are usually used to treat Diagnosis X, if they had symptoms consistent with Diagnosis X, I believe them and diagnosis X.
So here's how treatment goes. Usually the patient has symptoms and the majority of the time the symptoms are consistent with a specific diagnosis and everyone agrees. Let's say the diagnosis is recurrent major depression, moderate in intensity, coded 296.32. I start the patient on medications for this condition and they come for therapy. A few weeks go by, and the patients symptoms get better, but they still have issues going on in their life. Stressful things that they are dealing with, or troubling relationships, or life just not going the way they'd like, so they still come for therapy. And each visit, a bill is generated and the bill needs a diagnosis, so the diagnosis remains, because this is what is being treated and this is what the patient is getting medications for, and so it's 296.32, even if the patient's symptoms are at bay, or even if the patient comes in saying that they are anxious today, or even if the patient spends the entire session talking about the fight they had with their sister and never mentions a word about their mood or symptom complex. The diagnosis is usually a stable thing for the paperwork issues that call for it. I mentioned statements for insurers, but in clinics, it needs to be on treatment plans, and in EMRs, and any form that goes to an agency which has regulations, including Day Programs, Psychosocial Rehab programs, Care provider organizations, etc. No diagnosis, no services. And some services are only accessible to the patient with specific diagnoses that indicate a severe and persistent psychiatric illness. I would say that for a patient who has had numerous psychiatric hospitalizations, is unable to work, gets benefits from the government because they are disabled by mental illness, and requires medication to remain well, it seems reasonable to agree that a major psychiatric disorder exists, even if on a given day, the patient says he is not having any symptoms of the illness and is feeling well. It has to be this way, or no therapy would ever be done: every session would be a diagnostic evaluation with check lists of symptoms. Now I'm not saying that diagnoses never change...they do...people get manic and we realize that their unipolar depression is really bipolar depression, or with time we realize that there is more than one diagnosis, or that a preliminary diagnosis was simply wrong, or that alcohol or drugs were a bigger contributor to the symptom complex than we realized at first.
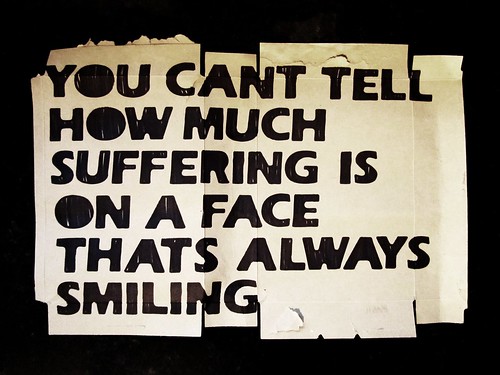
But when our theoretical patient, the one with major depression, moderate, who had a long hard course with it, notes that a long time has gone by with no symptoms of the illness (on medications and with therapy) and he asks, "So do I still have depression?" it does make for an interesting session.
What do you think?